The future of infertility medicine
Science is making great strides in creating germ cells, like sperm and eggs, in the lab. This research has been instrumental in under- standing how reproduction works, leading to new discoveries about the causes of infertility and possible treatments.
In October of last year, scientists from Kyushu University (Hikabe et al., 2016), Japan, reported the first direct creation of eggs from mouse iPS cells. Previously, mouse iPS cells had been used to create primordial germ cells (PGCs), which are the progenitors of sperm and eggs, but to acquire actual germ cells, the PGCs had to be injected into the ovaries of a mouse. The research from Kyushu goes a step further by showing how to acquire eggs without any animal transplantation.
Around the same time, the World Health Organization (WHO) released new criteria for the definition of infertility: couples that have tried but failed to conceive for at least one year. Some sources reported that the WHO extended this definition farther to include people who want children but are without partners, a claim the WHO has denied.
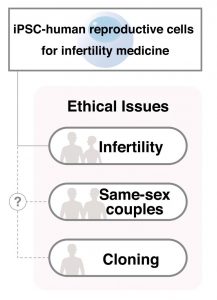
The incident brings to light questions about who has the authority to decide the definition. It is almost a certainty that in the future iPS cells will be used to make human reproductive cells for infertility medicine. While it is safe to assume that infertile couples will be eligible for this treatment, which other demographics will qualify remains debatable. Same sex couples, individuals without partners, and women beyond an age where they can conceive are all examples. These arguments will depend on what rights society de- cides people have to children.
Current science is still a long way from germ cells derived from human iPS cells, and iPS cell research has taught us that mouse cells are much easier to manipulate than human cells. Nevertheless, what has been accomplished in mouse cells has proven true for human cells in most cases, and it is thought to be only a matter of time until the exceptions disappear. Therefore, it is not pre- mature to begin consideration of our definition of infertility and which patients will have access to future infertility medicine.
By Dr. Tsutomu Sawai
